Non-Celiac Wheat Sensitivity: Why ATIs, Not Gluten, Could Be the Real Problem
When people experience bloating, fatigue, or the dreaded "brain fog" after eating a bowl of pasta or a sandwich, gluten is almost always the immediate suspect. It has become the dietary villain of the decade. But what if the real culprit isn't gluten at all? What if it is something else entirely, hiding in plain sight within the wheat grain?
Meet Amylase-Trypsin Inhibitors (ATIs)—a family of naturally occurring proteins in wheat and related grains that may be the true drivers of symptoms for the millions of people who believe they have "gluten sensitivity." Recent groundbreaking research suggests these proteins can trigger inflammation and gut discomfort even in those who test negative for celiac disease or wheat allergy.
What Are Amylase-Trypsin Inhibitors (ATIs)?
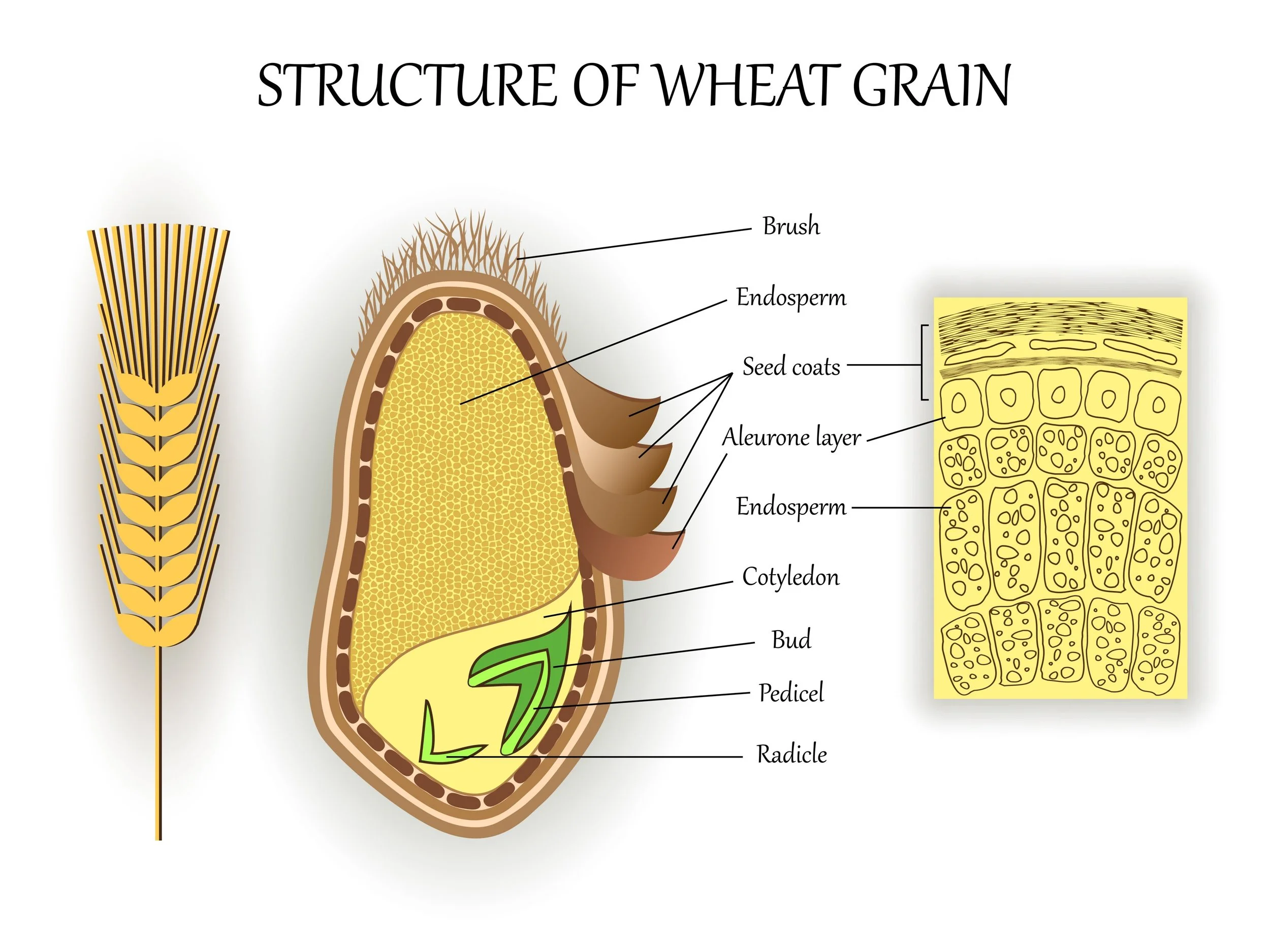
ATIs are small, resilient defense proteins found in the endosperm of grains like wheat, barley, and rye. Their evolutionary purpose is to act as a natural pesticide: they protect the plant from pests such as insects and fungi by blocking their digestive enzymes (specifically amylase and trypsin), effectively starving the attacker.
Wheat grain structure
But inside the human body, ATIs appear to do something far more reactive than simply inhibit digestion.
Researchers have discovered that ATIs can activate the innate immune system—specifically by engaging the Toll-like receptor 4 (TLR4) complex, a key sentinel of the body's immune response. This activation can trigger a cascade of low-grade inflammation in the gut and beyond, manifesting as the very symptoms—joint pain, fatigue, and bowel distress—that non-celiac patients often report (PubMed—https://pubmed.ncbi.nlm.nih.gov/25925932/).
In short: ATIs may help explain why some people feel better on a gluten-free or wheat-free diet—not because they are removing gluten, but because they are removing these immune-stimulating proteins.
The Science: How ATIs Trigger the Immune System
Unlike celiac disease, which is an autoimmune reaction driven by T-cells responding to gluten, the reaction to ATIs is an innate immune response. This distinction is critical because it means the mechanism of harm is fundamentally different.
Innate Activation: Studies show that ATIs from wheat directly activate innate immune cells (monocytes, macrophages, and dendritic cells) via the TLR4 pathway, driving intestinal inflammation (PubMed—https://pubmed.ncbi.nlm.nih.gov/27993525/).
TLR3 activation
Beyond the Gut: This inflammatory signal doesn't just stay in the intestines. It can travel to other parts of the body, potentially exacerbating other inflammatory conditions like fatty liver disease or even neuroinflammation (PubMed—https://pubmed.ncbi.nlm.nih.gov/32878020/).
Resistance to Digestion: Like gluten, ATIs are highly resistant to our own digestive enzymes, meaning they arrive in the intestine largely intact and biologically active, ready to interact with the immune system (Springer Link—https://link.springer.com/article/10.1007/s00394-022-02841-y).
Foods That Contain (and Don’t Contain) ATIs
If you suspect ATIs are your issue, the dietary strategy is remarkably similar to a gluten-free diet, but the reason is different. ATIs are found in the same gluten-containing grains, but they are absent in others.
High in ATIs (Avoid):
Wheat (all varieties: modern, spelt, kamut)
Barley
Rye
Triticale
Processed foods made with wheat flour
Low / No ATIs (Safe):
Rice
Corn (Maize)
Oats (Pure, uncontaminated)
Quinoa
Legumes (Beans, lentils, soy)
Note on Ancient Grains: While some ancient wheats like einkorn may have lower overall ATI activity compared to modern high-yield wheat, they still contain these proteins. For highly sensitive individuals, even ancient wheats might trigger a reaction (MDPI—https://www.mdpi.com/2072-6643/12/12/3785).
The Bottom Line: Rethinking Your Sensitivity
If "gluten" seems to upset your stomach, but celiac tests come back negative, you aren't imagining it. You might simply be blaming the wrong protein. ATIs—the plant's own pest-defense system—could be mounting a defense against you.
Recognizing ATIs as a potential cause validates the experience of "Non-Celiac Wheat Sensitivity" (NCWS) as a real, biological condition, not a fad. By choosing ATI-free grains like rice, corn, and oats, you can often achieve the same symptom relief as a gluten-free diet, but with a better understanding of why your body is thanking you.