The Chronology of Digestive Discord: How Our Biological Clocks Govern IBS
The rhythmic oscillation of life is often taken for granted until it begins to falter. For the individual navigating the complexities of Irritable Bowel Syndrome (IBS), the focus is naturally directed toward the immediate—the sharp pang of abdominal pain, the sudden urgency, or the persistent bloating. Yet, emerging science suggests that the seat of the problem may not reside solely in the intestines, but in the delicate internal clocks that govern our existence. We are beginning to understand that the gut does not function in a vacuum; it is part of a grander chronological scheme, and when our sleep-wake cycles drift away from our biological requirements, the digestive system often bears the brunt of the discord.
The Conductor and the Peripheral Orchestra
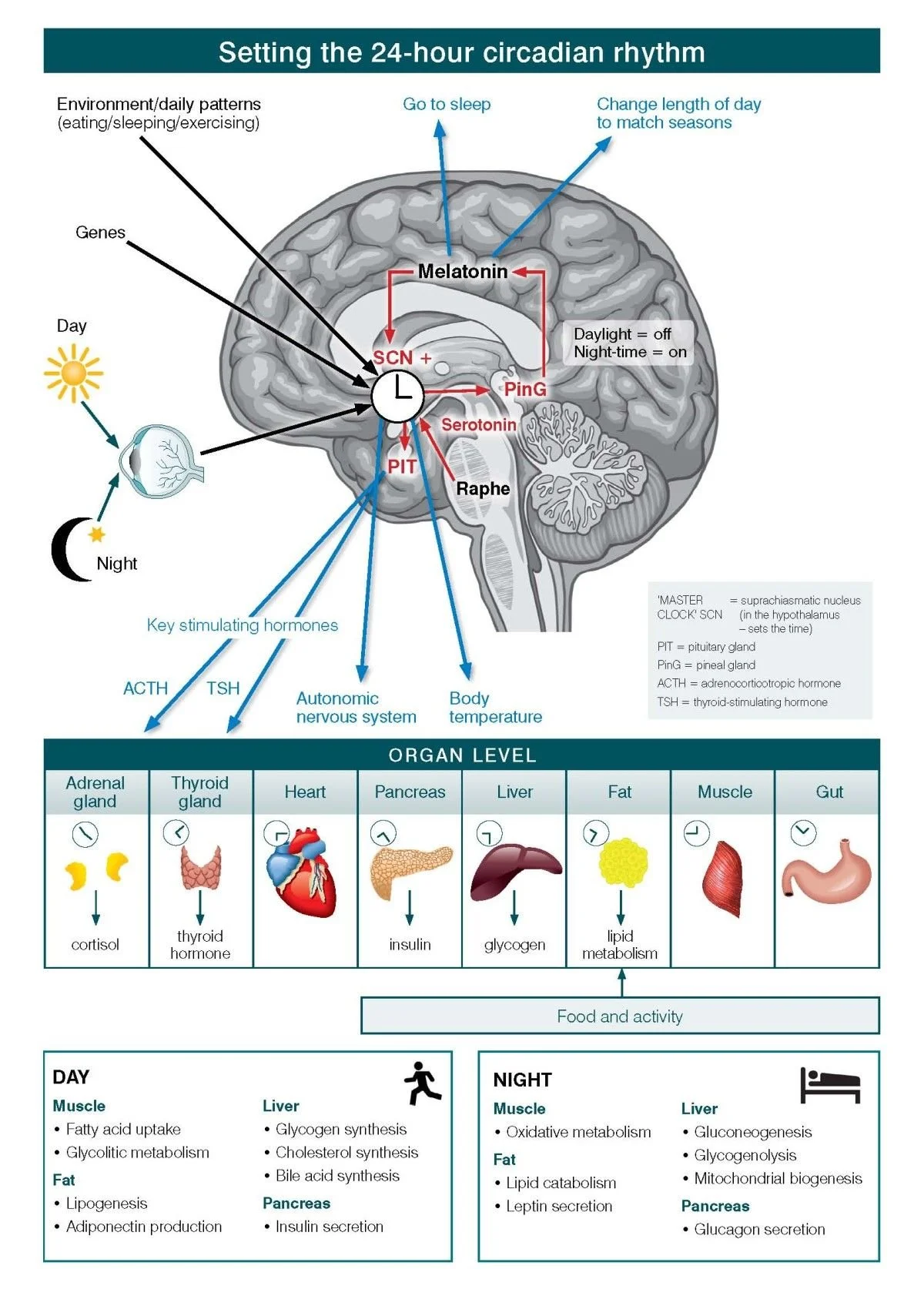
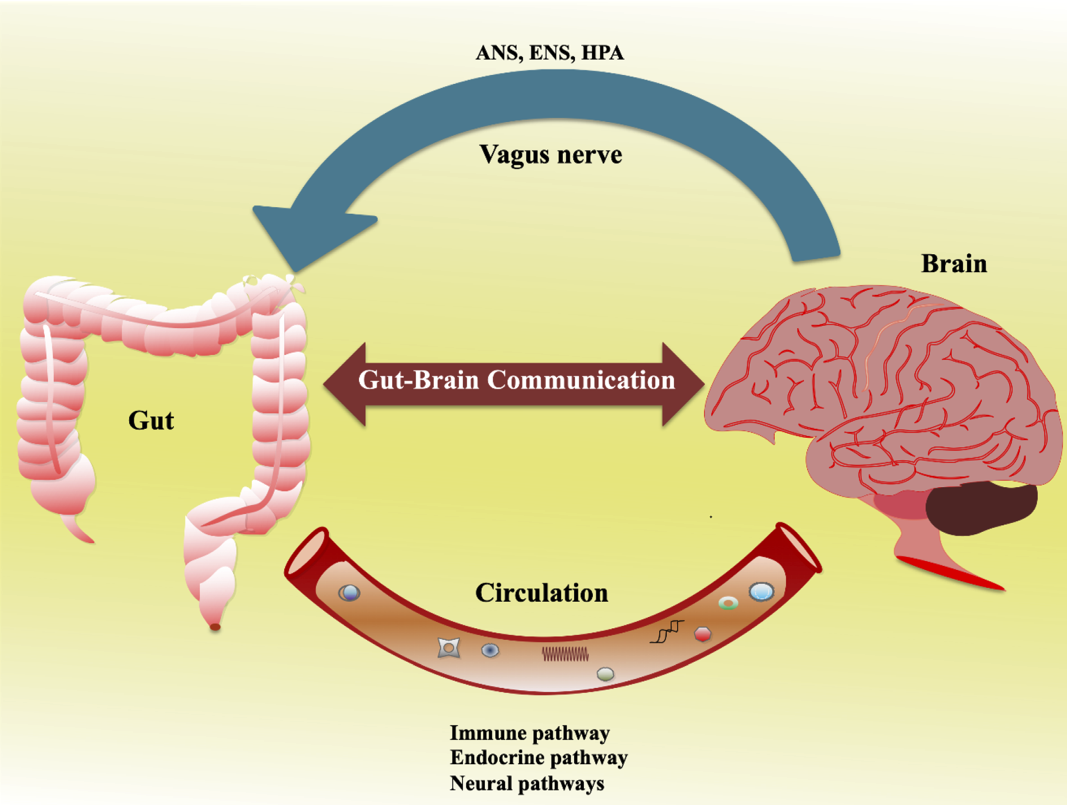
Sleep alignment refers to how closely an individual’s daily behavior matches their internal circadian clock. This system is orchestrated by the suprachiasmatic nucleus, or SCN, in the hypothalamus, which acts as the body's master pacemaker. However, as noted in (Nature Communications), the gut possesses its own autonomous "peripheral clocks" located within the epithelial cells and smooth muscle. These local timekeepers dictate essential functions including gastric emptying, intestinal motility, and the structural integrity of the gut barrier. While IBS is primarily a functional disorder of gut-brain interaction, it is useful to distinguish it from Inflammatory Bowel Disease (IBD). Whereas IBD involves visible, chronic inflammation of the digestive tract, IBS is often characterized by a desynchronization of these signaling commands rather than overt tissue destruction.
When sleep timing becomes irregular—a phenomenon researchers call "social jet lag"—these gut clocks become desynchronized from the brain's central commands. Investigation in the (Journal of Clinical Sleep Medicine) indicates that this temporal chaos can lead to increased gut permeability and a shift in the delicate microbial populations. For those with IBS, this is particularly precarious. The disruption of the Migrating Motor Complex, the "housekeeping" wave of the digestive tract that occurs during rest, can lead to the erratic bowel habits that define the condition. In this light, a late night is not merely a cause of morning fatigue; it is a physiological insult to the intestinal environment.
The Amplification of Visceral Pain
The relationship between sleep and the gastrointestinal tract is less of a linear progression and more of a complex, bidirectional feedback loop. Traditionally, IBS has been categorized as a breakdown in the communication between the brain and the gut. Recent investigations published by the (National Institutes of Health) underscore that this interaction is heavily regulated by circadian rhythms. One of the most significant consequences of poor sleep is the lowering of the visceral pain threshold.
This hypersensitivity is often mediated by the hypothalamic-pituitary-adrenal (HPA) axis and changes in serotonergic signaling—the same pathways targeted by many modern IBS therapies. By failing to secure restorative sleep, the patient inadvertently turns up the volume on their own physical discomfort. This intersection of sensory processing and rest is explored further in our discussion on Understanding the Gut-Brain Axis in IBS.
Melatonin as a Temporal Bridge
Melatonin, often narrowly defined as a "sleep hormone," serves as a crucial bridge in this temporal divide. While synthesized in the pineal gland to signal darkness, melatonin is produced in vastly greater quantities within the intestinal tract. Here, it acts as a powerful antioxidant and a regulator of motility. IBS patients frequently exhibit abnormal melatonin secretion patterns, which may contribute to both their sleep disturbances and their bowel symptoms. According to the (World Gastroenterology Organisation), restoring these biological rhythms can normalize bowel habits and improve quality of life even without radical dietary changes. Furthermore, research in (Mayo Clinic Proceedings) has explored how exogenous melatonin can significantly reduce abdominal pain scores in those suffering from functional digestive disorders.
Strategies for Restoring Biological Rhythm
Addressing this misalignment requires a shift in how we view treatment. It is no longer sufficient to focus solely on what one eats; one must consider when one eats and when one sleeps. "Chrononutrition"—the practice of aligning meal times with circadian rhythms—is becoming a pillar of functional GI health. Consuming large meals late at night forces the gut to remain active when it is biologically programmed to repair itself. Maintaining a strict sleep-wake schedule, seeking morning sunlight to anchor the master clock, and allowing for a sufficient fasting window before bed are not merely lifestyle "tips"; they are biological imperatives.
By viewing sleep not as a luxury, but as a core pillar of gut health, we move toward restoring biological resilience in both the brain and the gut. For those seeking to build these habits, our guide on Foundational Strategies for IBS Management provides a structured approach to integrating these habits into a daily routine. In the end, the goal is to move the body from a state of constant emergency back into its natural, quiet cadence.